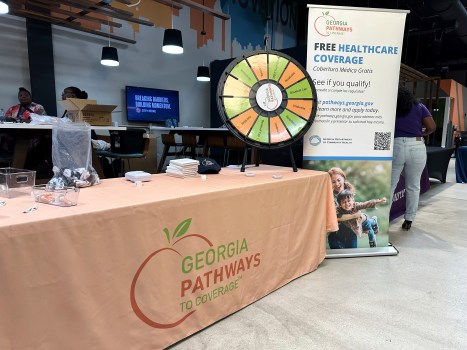
The government program known as Medicaid is designed to assist the underprivileged in paying for medical treatment. In recent years, its cost to taxpayers has increased dramatically, and by 2025, it will account for over 12% of federal tax income.
Medicaid was projected to spend $8.2 trillion in 2025–2034 (prior to the One Big Beautiful Bill), which is $2.7 trillion more than it would have if it had increased in line with inflation and population growth.
Medicaid was a state-by-state program prior to the Affordable Care Act (Obamacare), and it frequently only provided coverage to a fraction of those living below the poverty line, particularly mothers and children, but not typically working-age, work-capable adults. States were permitted by the Affordable Care Act to extend Medicaid to all individuals below the poverty line and those above it, irrespective of their circumstances. For those who became eligible as a result of the ACA expansion, 90% of the costs are covered by the federal government.
Then, under the Biden administration, the president and Congress worked together to weaken program integrity maintenance, make enrollment simpler, and make disenrollment more difficult. Enrolling and maintaining ineligible individuals had few consequences for states and private companies that provided insurance to beneficiaries. Consequently, taxpayer funds were improperly transferred to the coffers of insurance companies, states, and healthcare providers. This contributed significantly to Medicaid’s growth.
This accumulation threatened to displace other objectives by undermining Medicaid’s primary goal of assisting those who are most in need and making the program less affordable for taxpayers. In order to reduce misuse and put the program back on track to provide care for those who need it most, Congress incorporated modifications in the One Big Beautiful Bill.
This objective is partially achieved by the new employment requirements for Medicaid beneficiaries. It is a sensible change to require able-bodied individuals to work in order to be eligible for this taxpayer-funded benefit. Beneficiaries who are pregnant, disabled, have children, are elderly, have children under the age of 14, or are caregivers for others are exempt from the job requirements. Only states that have recently expanded Medicaid must meet the rules, which are specifically designed to target working adults.
The labor requirements are expected to aid in the detection and elimination of abuses such as the 2.8 million duplicate enrollments found by the Centers for Medicare & Medicaid Services. Deliberate or accidental fraudulent enrollment will be significantly more difficult to maintain due to work requirements.
Because officials felt that individuals who could work should work and save the safety net for those who couldn’t, states refused to cover capable adults prior to the Affordable Care Act. By default, it was a necessity for the job.
To ensure that benefits reach the most vulnerable and at a cost that is affordable for taxpayers, the Medicaid program urgently needs to be reformed. Work requirements support that objective without jeopardizing access for individuals who require it.
Economist and senior fellow Jeremy Nighohossian works at the Competitive Enterprise Institute.